How Involved Is Your Staff in Patient Collections?
It wasn’t that long ago that most practices left everything to do with billing to professional billers. Even patient collections were often managed entirely by the billing department (or the billing service). But health insurance and the revenue cycle have changed dramatically in recent years.
Did you know that one in three privately insured Americans have received a surprise medical bill because their health insurance covered less than they had expected? Did you also know that most insured patients now face some sort of deductible, and that nearly 40% of patients under 65 have HDHPs (high deductible health plans, defined by the CDC as plans with deductibles of more than $1,200). This means that for many patients, insurance won’t be paying a penny of the cost of services you render. On some plans, even office visits must be paid entirely by the patient until the deductible is met.
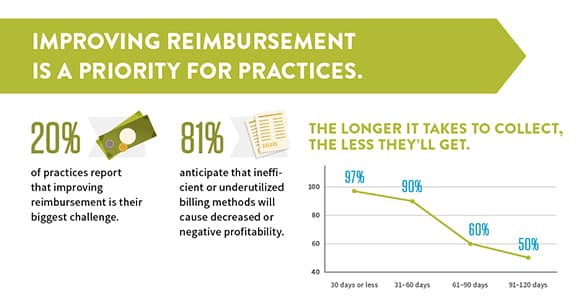
Bottom line is that patient responsibility for the cost of care has surged. Considering the large amounts patients now typically owe, plus the challenges of collecting post-service, you’re almost surely leaving a lot of money on the table if you and your staff aren't taking an active role in patient collections.
Let's consider an all too typical scenario: the patient receives the services they were looking for and leaves your practice without considering any financial implications – until the bill from your practice arrives. That bill (which arrives many weeks later, after insurance processes the patient’s EOB) comes as a complete surprise to the patient. Depending on the type of service your practice provided, the bill could be a very big surprise.
Several things could happen next, and most of the possibilities involve a cost to your practice. If the patient is surprised and confused, it’s not likely she’ll just pay the bill, especially if it’s large. But some might—that’s the best possible outcome. Most patients who are surprised will either call your practice for an explanation or to complain – and that means a cost to your practice in lost staff time, and perhaps even an unraveling of the relationship, if the patient becomes very upset.
Other patients will ignore the bill, convinced that it’s a mistake or hoping that insurance will end up paying it somehow. Your billers will respond by sending multiple statements over several months (each with a significant administrative cost attached). Some of those statements will not prompt any payment at all.
Delaying conversations with patients about financial responsibility will inevitably mean that some patients are surprised by their bills, like in this scenario. Some of those patients won’t pay in full or simply won’t pay at all; even when patients do pay, sending multiple statements and dealing with phone calls adds significant collection costs.
Starting the conversation before the patient visits your practice is the best tool we have to avoid surprising patients with bills they may be unwilling or unable to pay. To help your practice collect effectively from patients while also maintaining positive relationships, scheduling and front desk staff must play key roles in the process.
In my webinar, Navigating A New Era of Patient Collections, I discuss the scope of the patient payment challenge and some ideas for how your practice can collect more effectively.