3 Ways to Make eVisits Better
Is there a way to make eVisits Better? The recent report on eVisits from Deloitte & Touch shows that after decades of unfulfilled promise, 2014 is the inflection point of eVisit usage, with nearly 100 million eVisits this year alone - 75% of that in North America. OK, you knew that, yet there are still 3 primary problems with traditional eVisits -
i) Lack of provider enthusiasm.
ii) Long reply times from providers (doctors and staff).
iii) Lack of holistic answers to patients.
(Plug Warning: screenshot above is from a typical "Message Collaboration Solution" using DoctorBase technology).
Challenge #1) Lack of Provider Enthusiasm

While being attacked (unfairly IMHO) in the press/social-media for being slow to adopt technology, doctors do increasingly accept patient emails without reimbursement.
Sure, there's a CPT code for getting reimbursed for email on some health networks, but considering it takes 5+ minutes of a biller's time to account for one 45 second email - most say, "Forget it!"
Yet, websites like HealthTap (B2C - available to the public) and DoctorBase (B2B - available to organizations to host privately) have shown that doctors are willing to answer for Social Currency alone.
But yes, payment (in actual currency) would be nice too.
So whose going to pay?
CMS is considering how to reimburse for eVisits this year, but since it's now open for comments, don't expect any decisions this year. And while more and more case studies on eVisit implementation are increasing, 3 models are emerging:
A) Build it into the cost of the premiums/services:
Kaiser Permanente and One Medical do this well, as well as higher end services like Discover Health in San Francisco.
Traction: They've become market leaders in their segments and hyper-locations.
B) Charge patients a per message or monthly fee:
Doctors on Demand, HealthTap Prime and a host of other startups are entering this space.
Traction: TBD. I suspect, however, that the consumer acquisition costs of over $50 per patient that generates $40 per message requires tons of VC capital to create a brand that will lower those acquisition costs. Otherwise, it doesn't make financial sense as a business.
C) Direct to Employer:
As insurance costs go up (ours have nearly doubled in the last 3 years while being healthy twenty and thirty-something year old engineers) selling "Virtual Provider Networks" to augment health insurance plans form large employers or self insured employers are increasing. Here in San Francisco, it is becoming increasingly popular for startups to add these types of plans as a "perk."
Traction: More traction than charging patient directly, mostly because the sales process for selling direct to employers has a lower overall cost of customer (patient) acquisition.
POTENTIAL SOLUTION?
Social Currency is great for doctors to build SEO and Reputation Marketing points - as well as help the public - yet as John Malkovich's character said in the movie Rounders, "Pay the man."
Challenge #2: Long Wait Times for Replies
Forget it, I'll just go to WebMD and self-diagnose.
As I predicted in 2012, the Deloitte report on eVisits confirms that videoconferencing, Skype or Google Hangouts is minimal for eVisits (lack of time concurrency is extremely difficult for today's technology to solve). Most eVisits are done through simple messaging, yet the delays in receiving even a simple response, as reported by ComputerWorld can be 24 hours or longer.
There is simply no way that singular point-to-point or person-to-person secure messages can work to make reply times faster without painful (costly) changes to staff scheduling. But social media platforms like Yammer and Facebook have taught us that the power of group messaging can be extremely efficient - just post your next photo on Facebook and time how quickly you get your first comment/Like.
What we've seen at DoctorBase is that there are also surges and lulls in patient and doctor eVisit activity, and when patients ask questions versus when doctors are likely to answer are not always congruent throughout the week.
Collaborative group messaging has been around for over 10 years in the enterprise, but is just now coming into vogue in healthcare. This means that while a patient asking a question can have their existing provider respond, they can also opt to receive answers from a variety of other specialists and providers that are "in-network."
"This means that many patient questions on "Virtual Provider Networks" get answered within 30 minutes with multiple healthcare providers responding per question)."
POTENTIAL SOLUTION?
Replace or augment existing point to point secure messaging solutions with a 'Virtual Provider Network' (VPN) that allows existing patients to sign up for the service (and add their payment info if need be) then have the question go to the 'virtual team.' Without changing scheduling or much training, you'll see something amazing happen -
The 'Crowd in the Cloud' takes care of the patient without much bureaucracy or training. But yes, both of these things are good and needed when rolling out VPNs or eVisits of any kind; though VPNs require much less operational expense to deploy.
Patients just don't get answers an order of magnitude faster, but the answers from providers build on previous answers and often come from multiple specialists to give patients a much more thorough, holistic answer.
Challenge #3: Answers From Doctors Are Too Short.
The new "take two aspirin and call me in the morning" is email.
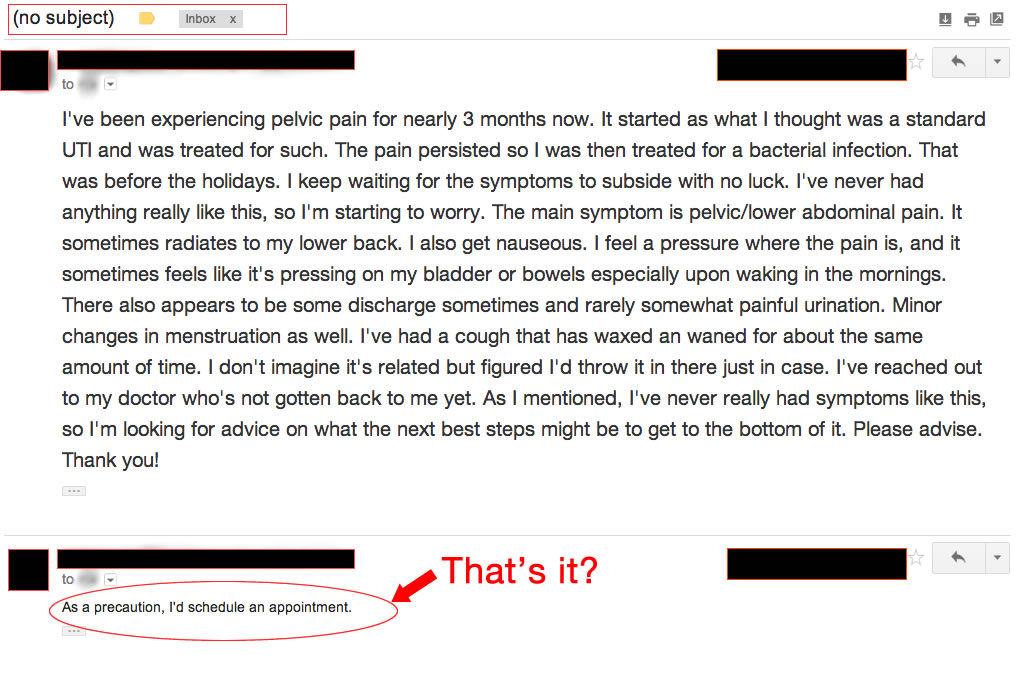
Doctors are short on time in world that calls for "care teams" and "care clouds" and "care synching," and - whatever other buzzwords for collaboration are floating around at conferences today. Yet most of the technology solutions available -
i) Don't integrate into legacy systems without substantial IT consulting.
ii) Require behavior changes in the staff (good luck).
iii) Are very expensive.
Still, they don't address the two primary psychological motivators behind giving longer, more thoughtful answers to patients -
i) If I give you a short and pithy answer - who but the patient will know?
ii) What's my motivation?
Effective Message Collaboration (secure messaging formatted to look like social media), instead of point-to-point secure messaging (which is just email behind a firewall) does two things -
1) It lets healthcare providers answer patient questions as part of a team - with the same ease of use as Facebook (yes, Message Collaboration can be HIPAA compliant).
2) Knowing that a provider's peers are going to read their answers to help construct their own responses to patients, Message Collaboration provides psychological incentives for doctors to provide more thoughtful, meaningful answers that try to address the patient issues within the communications stream - as opposed to just "getting through my emails."
* It would also allow hospital and health plan executives to provide bonuses and awards to doctors who are voted by their peers as consistently providing the "best" answers, are the most active, etc. It's a fantastic tool for Physician Alignment and Doctor Engagement.
Now....
The "rug that ties the room together" (I've been dying to use a Big Lebowski reference) -
Secure Message Collaboration creates Virtual Provider Networks that, with little cost or cutover pain, result in eVisits that lead to higher patient satisfaction and reduced opex costs.
So like, chill out man. It's all good.















